TOP 10 NUTRITION AND LIFESTYLE TIPS TO RELIEVE ACID REFLUX
Estimated reading time: 8 minutes
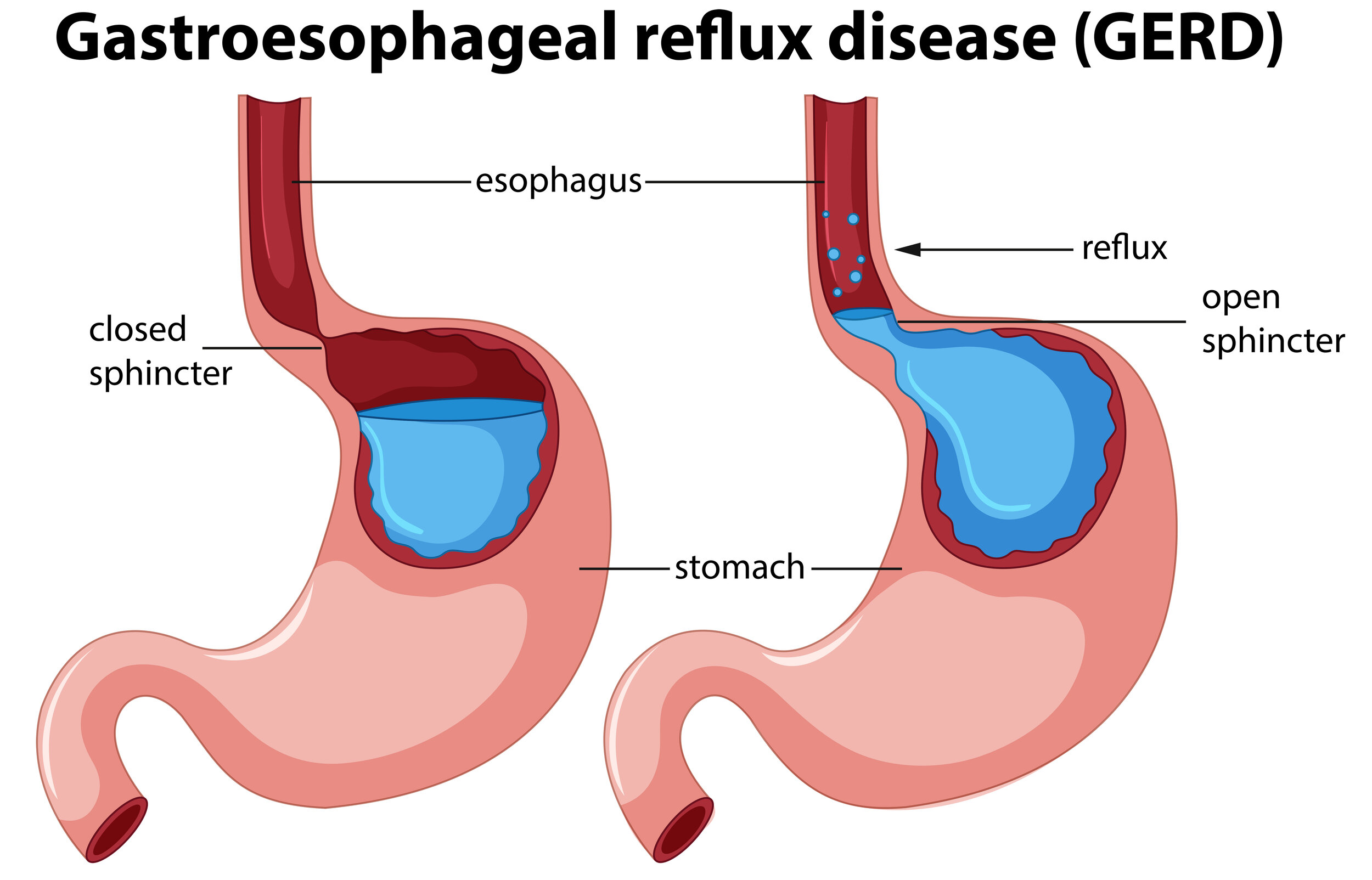
Acid reflux is very common. It occurs when stomach acid backs up into the oesophagus irritating the tissue.
Gastroesophageal reflux disease (GERD) is the chronic, more severe form of reflux. It is estimated that approximately 9% - 26% Europeans suffer with GERD (1).
Heartburn is the most common symptom of acid reflux, affecting up to 25% of UK adults (2).
OTHER SYMPTOMS OF ACID REFLUX
Regurgitation
Burning
Difficulty swallowing
Chronic bad breath
Chest pain
Nausea
Gas & bloating
Chronic sore throat
Excessive salivation
WHY DOES ACID REFLUX HAPPEN?
Located in the centre of your chest, the lower oesophageal sphincter (LES) is a muscle that separates the oesophagus from the stomach. Think of it like a fist. When you’re eating, it should be open and loose, to allow food to pass to your stomach. But at all other times the sphincter should be tightly closed to prevent all food and digestive fluids from the stomach travelling upward.
The secretions of the stomach are acidic; they are supposed to be. The main one is hydrochloric acid (HCL). HCL helps break down proteins & kills ingested bacteria and pathogens to prevent infection. HCL is so acidic, that if you put it directly on your hand, it would burn you. Another key component is digestive enzyme called pepsin that breaks down protein. HCL activates pepsin.
Your stomach is lined with protection from these acids, but your oesophagus is not. The delicate mucous lining in this part of the body can only take so much exposure. Too much acid for too long can cause irritation, inflammation & ulcers.
Acid reflux happens when LES is weak or relaxes inappropriately, allowing the stomach’s content to flow up into the oesophagus.
Acid reflux is caused by stomach acid in the wrong place.
NUTRITION & LIFESTYLE TIPS FOR ACID REFLUX
In most cases, this condition can be relieved through diet and lifestyle changes.
1. CHEW, CHEW, CHEW
The average person chews each bite of food only a few times before swallowing. Try to chew your food until it’s mostly liquid. This will make it easier for your stomach to break down your food.
2. DRINK MORE WATER, AWAY FROM MEALS
Water is incredibly important for your digestion (and health in general). However, too much liquid during meals can dilute your stomach acid and make it less potent, leading to bloating and belching. Food can stay in your stomach for longer than it should and ferment. This can cause gas to build up and put pressure on the LES that will eventually open, causing reflux.
Some water with your meals is ok. Healthy functioning digestive system can adapt its secretions to the consistency of a meal.
3. AVOID YOUR TRIGGER FOODS
Certain foods can be aggravating:
Spicy foods
Fatty foods
Fried food
Caffeine (coffee, tea, soda)
Carbonated drinks
Chocolate
Alcohol
Citrus juices
Tomato
Garlic & onion
Carminatives (mint and spearmint)
While studies are inconclusive (3,4), eliminating or at least dramatically reducing these foods while working on other root causes can often bring rapid relief. Do I think you should remove all of these from your diet? No! Should you experiment and see if any of these make your symptoms worse? Yes. Once symptoms go away, re-introduce one food at the time and monitor your symptoms.
4. CHECK FOR FOOD SENSITIVITIES
Beyond the LES relaxants & irritants listed above, the common sensitivities I see in my clinic are:
Dairy (5)
Gluten (6)
Soy
Many people with some form of grain or dairy intolerance report that they feel better when they remove these foods. Elimination diet is the gold standard. Working with a qualified health care provider is important as they can guide you in this process. They will also make sure that you are adding foods in, not just taking foods out, as this could lead to nutritional deficiencies.
5. EAT SLOWLY, UNTIL YOU ARE SATISFIED (NOT STUFFED)
Yes, it’s true that the stomach will stretch, but only so far. Too much food in our bellies can cause a temporary distortion of the LES. Give your stomach time to empty itself while you eat.
6. ADDRESS NUTRITIONAL DEFICIENCIES
MAGNESIUM
Low magnesium can cause LES muscle to be too tight or to spasm erratically. “Subclinical magnesium deficiency is a common and under-recognised problem throughout the world” (7).
ZINC
Adequate zinc levels are necessary for the production of HCL. Test, don’t guess! There are some easy and affordable ways to test your zinc levels. Speak to your Nutritional Therapist.
7. EAT YOUR LAST MEAL 2-3 HOURS BEFORE BEDTIME
Our muscles relax bit more at night, including LES. This can make reflux worse. If you have GERD at night, try elevating the head of your bed 4-6 inches (8).
8. AVOID TIGHT CLOTHING
Tight clothes around the stomach area can put tremendous pressure on your digestion and push your food and digestive secretions upward.
9. REDUCE STRESS, ESPECIALLY AROUND MEAL TIMES
Stress worsens GERD. Try to make mealtimes relaxing. When we are stressed (‘fight or flight’), our digestive secretions and peristalsis are noticeably reduced (by 30-60%).
Breathing exercises have been shown, to some extent, relieve GERD symptoms and improve pressure generated by LES (9).
Studies found stress to be one of the biggest factors worsening GERD symptoms. One theoretical explanation is that stress may cause changes in the brain that turn up pain receptors, meaning; we will feel the symptoms more, even if there is no change to the actual symptoms.
10. ACHIEVE & MAINTAIN HEALTHY BODY WEIGHT
There is accumulating data that obesity is associated with complications related to longstanding GERD such as erosive esophagitis, Barrett's oesophagus, and oesophageal cancer. “Central obesity, rather than body mass index (BMI), appears to be more closely associated with these complications.”(10)
Weight loss can help reduce &/or eliminate GERD symptoms. In one study, 81% of patients had reduction in symptoms, and 65% had complete resolution after completing a structured weight loss program (11).
OTHER POSSIBLE DRIVERS TO CONSIDER
HYPOCHLORHYDRIA
0therwise known as low stomach acid. The stomach can produce less acid as a result of ageing, It is also very common in those with chronic stress, thyroid & adrenal issues.
HELICOBACTER PYLORI
H. Pylori bacteria, when overgrown, has been shown to cause ulcers in the lining of the stomach or the upper part of the small intestine. It can also cause chronic GERD. This infection can also contribute to low levels of HCL, making the matters worse.
SMOKING
Research linked smoking to some of the worst complications of GERD, including throat cancer. Nicotine causes LES to relax, prompts the stomach to produce more acid (increasing the risk of gastric juices being refluxed into the oesophagus) & damages the mucus membranes that help protect the oesophagus from acid damage.
MEDICATION
Talk to your doctor or pharmacist about any medications or supplements you’re taking. Some may worsen reflux.
Unfortunately, the most common way of dealing with acid reflux often exacerbates it in the long run. Taking acid blocking medications does not address the underlying cause, and chronic use can lead to nutritional deficiencies. While weaning off Proton Pump Inhibitors (PPIs) is possible, you have to do so slowly and with the help of your doctor or other practitioner.
HIATUS HERNIA
One of the most common reasons for prolonged ongoing reflux.
SLEEP PROBLEMS
Lack of sleep has been shown to result in digestive problems, including reflux and GERD
While common and many people brush off the symptoms, GERD is a potentially serious condition and when left untreated, it can lead to other health issues and serious complications.
Image source: www.freepik.com
Written by: Jana Papajova
Published on: 16th May 2020
References:
1. El-Serag, H. Sweet, S. Winchester, C. et al. (2013). ‘Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review’. Gut, 63(6), pp.871-880.
2. Guts UK Charity. (2020). Heartburn and Acid Reflux. [online]. Available at: https://gutscharity.org.uk/advice-and-information/symptoms/heartburn-and-reflux/
3. Chumpitazi, B. Kearns, G. & Shulman, R. (2018). ‘Review article: the physiological effects and safety of peppermint oil and its efficacy in irritable bowel syndrome and other functional disorders’. Alimentary Pharmacology & Therapeutics, 47(6), pp.738-752.
4. Young, A. Kumar, M. & Thota, P. (2020). ‘GERD: A practical approach’. Cleveland Clinic Journal of Medicine, 87(4), pp.223-230.
5. Farahmand, F. Najafi, M. Ataee, P. et al. (2011). ‘Cow's Milk Allergy among Children with Gastroesophageal Reflux Disease’. Gut and Liver, 5(3), pp.298-301.
6. Usai, P. Manca, R. Cuomo, R. et al. (2008). ‘Effect of gluten-free diet on preventing recurrence of gastroesophageal reflux disease-related symptoms in adult celiac patients with nonerosive reflux disease’. Journal of Gastroenterology and Hepatology, 23(9):1368‐1372.
7. DiNicolantonio, J. O’Keefe, J. & Wilson, W. (2018). ‘Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis’. Open Heart, 5(1), p.e000668.
8. Khan, B.A. Sodhi, J.S. Zargar, S.A. et al. (2012). ‘Effect of bed head elevation during sleep in symptomatic patients of nocturnal gastroesophageal reflux’. J Gastroenterol Hepatol, 27(6), pp.1078-1082.
9. Pettit, M. (2005). ‘Treatment of Gastroesophageal Reflux Disease’. Pharmacy World & Science, 27(6), pp.432-435.
10. Ashrafi, D. Osland, E. & Memon, M. (2020). ‘Bariatric surgery and gastroesophageal reflux disease’. Annals of Translational Medicine, 8, pp.11.
11. Singh, M. Lee, J. Gupta, N. et al. (2013). ‘Weight loss can lead to resolution of gastroesophageal reflux disease symptoms: a prospective intervention trial’. Obesity, 21(2), pp.284-290.